Abstract

Introduction. The MIOT (Myocardial Iron Overload in Thalassemia) Network was a national Italian network constituted by thalassemia and magnetic resonance imaging (MRI) centers built in 2006. The main aim was to assure available, accessible homogeneous and standardized T2* MRI cardiac and liver iron overload assessments for a significant number of patients with emoglobinopathies. Moreover, the creation of a solid clinical-instrumental web based database allowed data exchange between centers and constituted a means of monitoring health care processes and outcomes. We describe the impact of this ten-year Network on cardiac complications in patients with thalassemia major (TM).
Methods. Among the 2497 emoglobinopathies patients consecutively enrolled in the MIOT Network we considered the 1401 TM patients who performed an end-of-study MRI. Per protocol the MRI follow up was scheduled every 18±3 months. Myocardial iron overload (MIO) was quantified by the multislice multiecho T2* technique. Biventricular function was quantified by cine images.
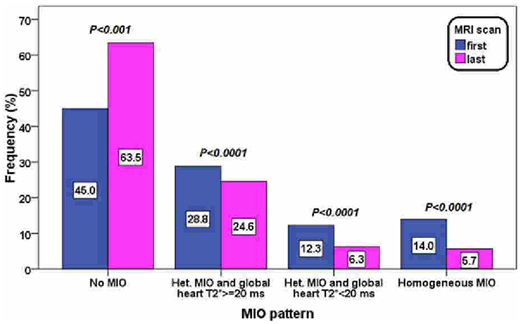
Results. At the last MRI significantly higher global heart T2* values (35.5±10.7 ms vs 29.2±12.0 ms; P<0.0001) and a significant lower number of patients with global heart T2*<20 ms (26.3% vs 12.0%; P<0.0001) were detected. Four patterns of MIO were identified: no MIO (all segments with T2*≥20 ms), heterogeneous MIO and global heart T2*≥20 ms, heterogeneous MIO and global heart T2*<20 ms, and homogeneous MIO (all segments with T2*<20 ms). Figure 1 shows the frequency of the 4 patterns at both scans. At the last MRI a significant higher frequency of patients with no MIO and a significant lower frequency for the other three patterns indicating MIO were detected. An improvement in MIO, that is a transition to a better risk class, was detected in the 68.4% of patients showing MIO at the baseline (at least one pathologic segment).
In patients with significant baseline MIO (global heart T2*<20 ms) a significant increase in left ventricular ejection fraction (EF) (mean difference: 3.2±8.5 %, P<0.0001) as well as in right ventricular EF (mean difference: 1.2±8.9 %, P=0.002) were detected with a concordant improvement of MIO status.
Based on MRI results the 75% of the patients changed the chelation therapy. At the last MRI the percentage of patients with an excellent/good compliance was significantly higher (94.7% vs 92.7%%; P=0.034).
The 13.1% of the patients had a cardiac complication (heart failure, arrhythmias, pulmonary hypertension, myocardial infarction, angina, myo/pericarditis, and peripheral vascular disease) before the enrolment in the project. During the study, the frequency of cardiac complications was 7.9 %, significantly lower (P<0.0001). In particular, the frequency of heart failure was significantly lower (5.9% vs 1.7%, P<0.0001).
Conclusion. Over a period of 10 years, the continuous monitoring of cardiac iron levels and a tailored chelation therapy allowed a reduction of MIO in the 70% of patients and a consequent improvement of cardiac function and reduction of heart failure. So, a national networking as the MIOT project was effective in improving the care and reducing cardiac outcomes of TM patients.
Pepe:Chiesi Farmaceutici S.p.A., ApoPharma Inc., and Bayer: Other: No profit support.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal